Mental health support for Long Term Health Conditions
Over 15 million people in England (30% of the population) have one or more long-term health conditions. There is a close relationship between long-term health conditions (LTC) and mental health and wellbeing.
Having LTC’s and mental health issues at the same time are highly common; an estimated 30% of all people with LTC’s also have a mental health problem. The likelihood of having depression and anxiety is higher in people with LTC’s compared to the general population. In a study of more than 245,000 people in 60 countries, up to 23% of participants with one or more chronic LTC also had depression.
Past experience, coping strategies, emotional resilience and health-related behaviours all influence the response to diagnosis and the impact of living with physical symptoms and resulting disabilities. The impact will change over time as the health condition, disability and circumstances change.
Types of health Conditions people have that we can support
- Type 1 and 2 Diabetes
- Chronic Obstructive Pulmonary Disease (COPD)
- Coronary Heart Disease (CHD)
- Chronic Fatigue Syndrome (CFS) / Myalgic Encephalomyelitis (ME)
- Fibromyalgia
- Chronic Pain (Muscular and Skeletal)
- Irritable Bowel Syndrome (IBS)
Group Treatments
- Cognitive Behavioural Therapy (CBT) Groups for LTC’s and Depression
- Discuss the impact a diagnosis of LTC’s on mood
- CBT models of depression
- Models of pain management and information about the nervous system
- Behavioural activation and pacing techniques, promoting value-based activities to boost mood (balanced living)
- Sleep hygiene
- Physical relaxation techniques appropriate to people with chronic pain,
- Cognitive restructuring (identify and challenge unhelpful illness beliefs)
Graded Exercise Therapy (GET) Group
NICE Guidelines recommend GET as one of the most effective therapies for CFS/ME
This treatment focuses on the use of regular physical activity to help clients feel less tired, improve fitness, and reduce difficulties in daily living. GET includes:
- Planning regular physical activity, to gradually increase the duration over time
- Impact of deconditioning and boom and bust cycles
- Strategies to recondition the body to break these vicious cycles
Computerised CBT (cCBT)
The Computerised CBT programmes use a combination of education and standard CBT techniques, such as worry management, activity planning and cognitive restructuring. They incorporate education about the specific conditions to help clients manage their mental health. The programmes are aimed at the following LTC’s:
- Chronic Heart Disease
- Chronic Pain
- Diabetes
- Lung Conditions
One-to-One CBT
- Diabetes: Using behavioural activation & activity planning to help the client manage their diabetes as well as cognitive restructuring around illness beliefs and adjustments to lifestyle.
- COPD: Uses psychoeducation, worry management an breathing techniques to improve quality of life and help clients see the difference between breathing difficulties to manage breathlessness. [Clients should also be offered pulmonary rehabilitation before CBT].
- CHD: Standard CBT treatments are used in addition to adjustments for unhelpful beliefs in relation to heart disease. [Cardiac rehabilitation should also be offered].
- Chronic Pain: Psychoeducation around the nature and function of pain. Use of pain cycles as well as pacing, activity planning and boom and bust cycles are used to increase quality of life and daily functioning.
In addition Step 3 CBT Therapists specifically treat more complex presentations of the above and the conditions below:
- CFS/Fibromyalgia: treatment involves high-intensity CBT techniques to manage thoughts and expectations around illness beliefs, manage energy levels by planning patterns of activity and rest, and manage sleep problems.
- Irritable Bowel Syndrome: high-intensity CBT treatment focuses on management of anxiety linked to stomach problems.
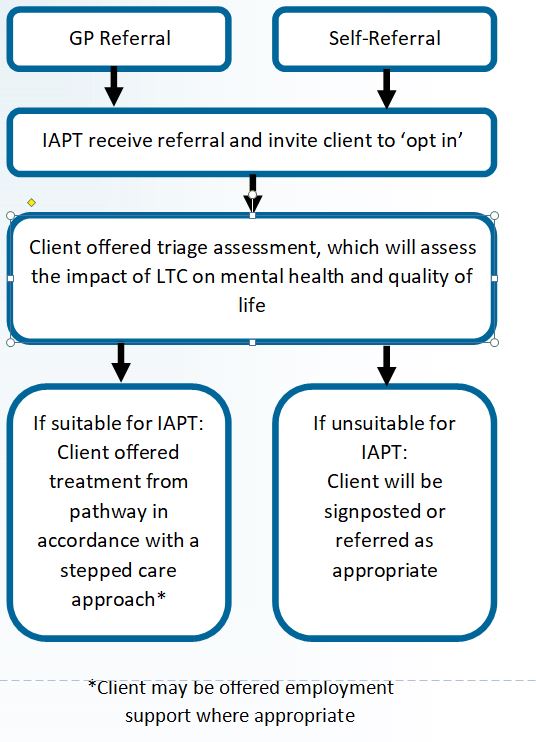
Referral Pathway